Good oral hygiene is an important factor in maintaining dental health for everyone, however, it…
Rule of thumb
Non-nutritive sucking habits are common in babies and young children, regardless of socioeconomic background, who do it for security and to comfort themselves. These can include the use of dummies, sucking of fingers, thumbs or even blankets.
The prevalence of these habits is greater in girls than boys and tends to reduce with age from a reported 30% at one year of age to 12% at nine years of age and then 2% at 12 years of age, as it becomes socially less acceptable. The good news is that most non-nutritive sucking habits cease spontaneously by the age of 4. However, the dentoavleolar and skeletal effects of such habits will depend very much upon their frequency, intensity, and duration.
We’ve all seen the effects that prolonged digit-sucking habits can have on the developing dentition:
- Proclined maxillary incisors
- Increased overjet
- Retroclined mandibular incisors
- Posterior crossbite
- Anterior open bite
- Upper anterior spacing
But the real question… is what is “prolonged”? How long is too long?
Studies show that there is spontaneous correction of the dental effects of digit sucking habits provided it stops by the age of 6 years old. So, the magic cut off age is 7, after which the position of the adult dentition is permanently affected and self-correction is less likely to take place.
As dental health professionals who see our patients on a regular basis, we are ideally positioned to intervene and encourage cessation early to reduce the deleterious effects of prolonged non-nutritive sucking habits.
So, how do we do this?
There are 2 approaches that can be used separately or in conjunction with each other, these are non-orthodontic and orthodontic interventions.
Non-orthodontic interventions:
- Consider using a dummy for younger children as it tends to be easier to phase out than a digit-sucking habit.
- Lots of encouragement and positive reinforcement perhaps with small rewards for milestones reached. Reward charts are available from many retailers, for example The Early Learning Centre, and parents may find the use of such adjuncts helpful.
- Physical barriers come in a multitude of shapes and sizes-plasters, gloves, thumb guards, and can benefit those who find themselves subconsciously placing digits in their mouths.
- Chemical deterrents, like “Stop ‘n grow”, have a bitter taste and have been shown to be an effective deterrent in cases on thumb sucking and nail biting.

Most of these methods are cost-effective and easily accessible to the public so can be very useful in the battle against non-nutritive sucking habits. However, they are still reliant on patient compliance.
Orthodontic Interventions:
If non-orthodontic interventions are unsuccessful, then fitting patients with a habit breaker may well be the answer, particularly in the 7-12 year age bracket when such appliances will be better tolerated.
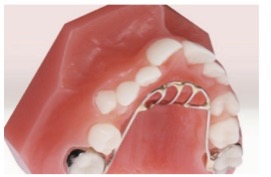
- Removable habit breakers can be used to discourage digit habits. The design tends to comprise of an acrylic base plate and retentive components, with a metal protuberance embedded in the acrylic hanging vertically down from the palate. These prevent patients from being able to place digits in their mouths comfortably. Their biggest flaw is that they are removable, so again, rely on patient co-operation.
- Fixed habit breakers may be the best option for patients who are struggling to break a digit habit. They can be of a similar design to the removable habit breakers, or perhaps a quadhelix, which can be used as an adjunct to comprehensive orthodontic treatment. Once fitted, fixed habit breakers should remain in situ for a minimum of 6 months to allow for maximum dental and vertical skeletal correction.
If non-nutritive sucking habits continue past 12 years of age, treatment becomes far more complex as the permanent dentition is fully established and tooth eruption complete. Such cases may require a combination of orthodontics and orthognathic surgery for ultimate correction of both dental and skeletal aspects of the resulting malocclusion.
So given the impact that digit habits can have for our patients, it should be a big THUMBS UP to helping our patients put their THUMBS DOWN.
